Collaborations: Prof Jane Pillow, Dr. MarJanna Dahl (University of Western Australia); Prof Lorenza Draghi (Politecnico di Milano, Department of Chemistry Material and Chemical Engineering)
Fundings: Telethon Perth Children’s Hospital Research Fund provided funding for the study
Congenital Diaphragmatic Hernia (CDH) is a fetal malformation resulting in incomplete closure of the diaphragmatic membrane. The resulting opening between the chest and abdominal cavities and the higher abdominal pressure allows herniation of abdominal organs into the chest interfering with the physiological lung development. Infants with CDH are at risk for pulmonary hypoplasia and pulmonary hypertension. The currently available prenatal treatment, fetal endoscopic tracheal occlusion (FETO), aims to reduce lung hypoplasia and hypertension occluding trachea with a latex balloon promoting Fetal Lung Fluid (FLF) accumulation into the lungs. Even if good results are proved, fetal tracheal occlusion prevents lung fluid in/efflux and fetal breathing and modify trachea structure. Despite increased lung volume, alveolar type II cell development is abnormal with a consequent reduction of surfactant production. Finally, the current clinical procedure mitigates this by removing the balloon at 33 weeks gestation by an additional surgical procedure that can promote preterm rupture of membranes (PROM).
To overcome these limitations new prenatal occlusion strategies are under study in a collaborative project between Politecnico di Milano and the University of Western Australia (UWA), approved by the Large Animal Ethics Committee at the University of Western Australia in October 2018. The aim of this project is to use and evaluate in a preclinical animal model the efficacy of a tracheal occlusion performed with a biodegradable self-dissolving hydrogel designed by Prof Lorenza Draghi, that should reduce the impact on the trachea and dissolves before birth, with no need for the second surgery for removing the plug.
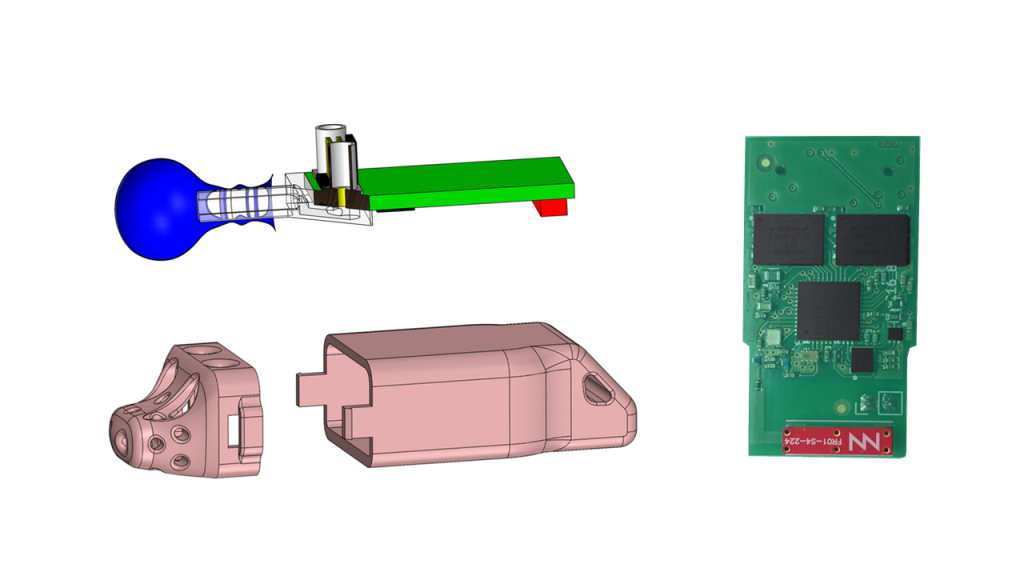
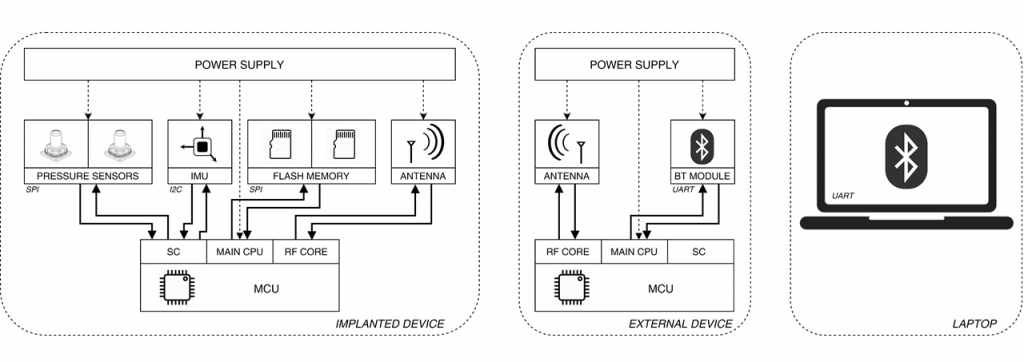
In this study our main contribution was double. First, we designed a new system for continuous lung pressure monitoring to quantify the occlusion impacts on the lung pressure and on FBM during the gestation since the occlusion is performed. The system is composed by two device, one external that acts as a transceiver and a second implanted in the amniotic sac to measure lung and amniotic pressure. The implantable device is based on a Microcontroller Unit (MCU), two pressure sensors, an Inertial Measurement Unit (IMU) to monitor fetal orientation, and an antenna to communicate data real time to the externa transceiver. It is encapsulated in a 3D printed shell that prevents direct contact with fluid with a resulting dimension of 72 mm x 29 mm x 19 mm. The total device life resulted equal to 58 days.
Secondly, our activity was concentrated on the assessment of afterbirth lung mechanical properties through the Forced Oscillation Technique (FOT). Measurements were performed twice: the first time in a few minutes after birth and the second time two hours later, to assess both the lungs characteristics but also to see the evolution in time.